The clock on the wall of Wetaskiwin Hospital’s diagnostic imaging department reads 6:17 a.m. as Jane Colby arrives for her CT scan. After months of unexplained symptoms and a referral that would have seen her driving to Edmonton multiple times, the 67-year-old farmer is visibly relieved to be just fifteen minutes from home.
“I used to dread these appointments,” she tells me, waiting in the newly renovated reception area. “My husband would have to take the day off to drive me into the city. Now I can be back home before the cows need feeding.”
Jane’s experience reflects a quiet revolution happening across rural Alberta’s healthcare landscape. Communities like Wetaskiwin, Camrose, and Drayton Valley are witnessing something remarkable – the arrival of medical technology previously available only in urban centers.
The Wetaskiwin Health Foundation recently completed a $1.8 million fundraising campaign to bring state-of-the-art CT scanning equipment to the local hospital. This achievement represents more than just new machinery – it symbolizes a reimagining of rural healthcare access.
“When we started this project, we heard countless stories of patients traveling hundreds of kilometers for basic diagnostic imaging,” explains Dr. Sarah Matheson, who has practiced rural medicine in Alberta for fifteen years. “For elderly patients or those with mobility challenges, these journeys could be physically and financially devastating.”
According to Alberta Health Services data, approximately 42% of the province’s population lives outside major urban centers, yet historically these communities have had access to less than 25% of advanced diagnostic equipment. The consequences of this disparity are measurable – Statistics Canada reports rural Albertans face up to 18% longer wait times for critical diagnoses and treatment.
The foundation’s executive director, Robert Callaghan, describes the community response as overwhelming. “We had everyone from school children to seniors’ groups participate. A local quilting circle raised over $7,000 selling handmade quilts at the farmers’ market. The community understood what was at stake.”
What makes this rural technology initiative particularly significant is its timing. Coming in the wake of the pandemic, which saw rural healthcare systems stretched to breaking points, these investments represent a commitment to addressing longstanding geographic inequities in medical access.
The morning I visit, the waiting room fills with patients from surrounding communities. Among them is Thomas Cardinal, a 34-year-old construction worker from a nearby Cree community who injured his back on a job site. “Before this machine, I was looking at taking three days off work for appointments in Edmonton,” he says. “That’s three days without pay my family can’t afford.”
His sentiment echoes findings from the Rural Municipalities of Alberta association, which documented how healthcare access challenges disproportionately impact Indigenous communities and lower-income rural residents who face compounded barriers of distance, transportation costs, and lost wages.
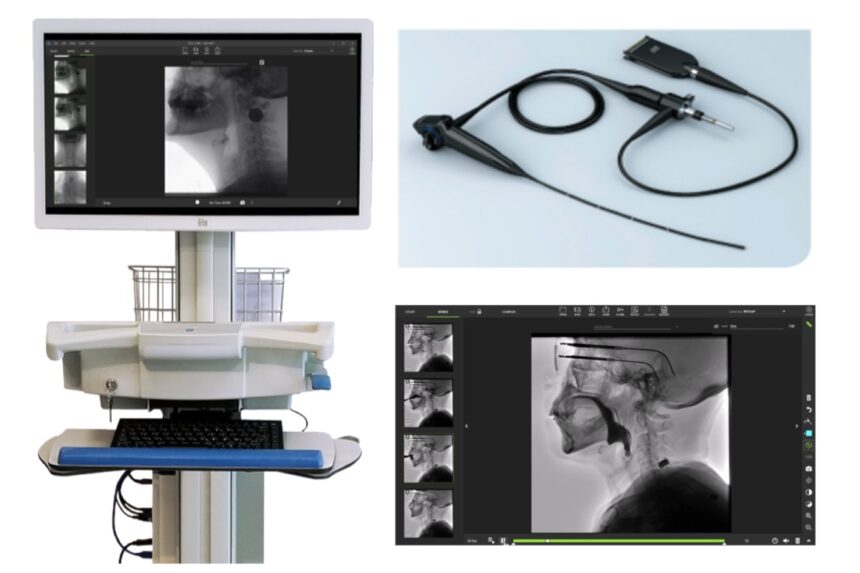
What’s happening in Wetaskiwin isn’t isolated. Similar community-driven initiatives are emerging across rural Alberta. In Drayton Valley, a foundation-led campaign recently funded portable ultrasound equipment that allows for bedside diagnostics in emergency situations. In Camrose, new ophthalmology equipment means seniors no longer travel to Edmonton for routine eye care.
Dr. Alim Nagji, who splits his practice between rural clinics and the University of Alberta Hospital, explains the broader implications. “When we bring advanced technology to rural settings, we’re not just improving convenience. We’re often catching conditions earlier, when they’re more treatable. The health outcomes data is starting to show significant improvements.”
Indeed, preliminary findings from Alberta Health Services suggest rural communities with enhanced diagnostic capabilities see up to 23% faster treatment initiation for serious conditions like cancer and cardiovascular disease.
The technology integration extends beyond hardware. New telemedicine platforms connect rural physicians with urban specialists in real time, allowing for collaborative diagnosis and treatment planning. Last month, a patient in Wetaskiwin received a complex neurological consultation with an Edmonton specialist who reviewed their CT scan minutes after it was taken.
These successes haven’t come without challenges. Healthcare staffing shortages affect rural facilities disproportionately. Wetaskiwin’s new CT scanner initially operated at reduced capacity until additional technologists could be recruited and trained.
“The equipment is only half the equation,” acknowledges John Beaton, Wetaskiwin Hospital’s administrative director. “We’ve had to get creative with staffing solutions, including partnering with NAIT’s medical radiation technology program to create rural placement opportunities for students.”
This approach appears to be working. Three recent graduates have accepted positions in rural facilities after completing placements there – a significant win for communities that have historically struggled to attract healthcare professionals.
Funding these initiatives requires innovative approaches too. While provincial healthcare budgets provide baseline operational funding, the capital investments for new technology increasingly rely on community foundations and private donors. This raises questions about equity and sustainability that policymakers are only beginning to address.
As the morning progresses at Wetaskiwin Hospital, I watch the careful choreography of patients moving through the diagnostic imaging department. A retired teacher receiving follow-up care for a heart condition. A teenage hockey player with a suspected concussion. A pregnant woman getting an ultrasound with her partner by her side. All receiving care in their community that would have been impossible just years ago.
Before I leave, I speak with Clara Jennings, a nurse who has worked in rural healthcare for over three decades. “The technology matters,” she tells me, “but what really matters is what it represents – the recognition that rural lives and rural health deserve the same standard of care as anywhere else.”
As rural Alberta communities continue advocating for healthcare equity, their success offers valuable lessons about the power of community-driven change. The revolution in rural healthcare may be quiet, but its impact promises to be profound and lasting.