As I walked into the empty waiting room of a family practice in downtown Charlottetown last Thursday morning, the silence felt loaded with meaning. Just two years ago, this same space bustled with patients flipping through dog-eared magazines while waiting to see their family doctor. Today, the practice sits dormant – one of 14 family physician positions currently vacant across Prince Edward Island.
“We’re operating in crisis mode,” Dr. Krista Cassell told me when I called her later that day. As the president of the Medical Society of PEI, she’s become the reluctant voice for physicians reaching their breaking point in Canada’s smallest province. “Doctors are exhausted, overwhelmed, and now feeling disrespected by government officials who don’t seem to understand the gravity of our situation.”
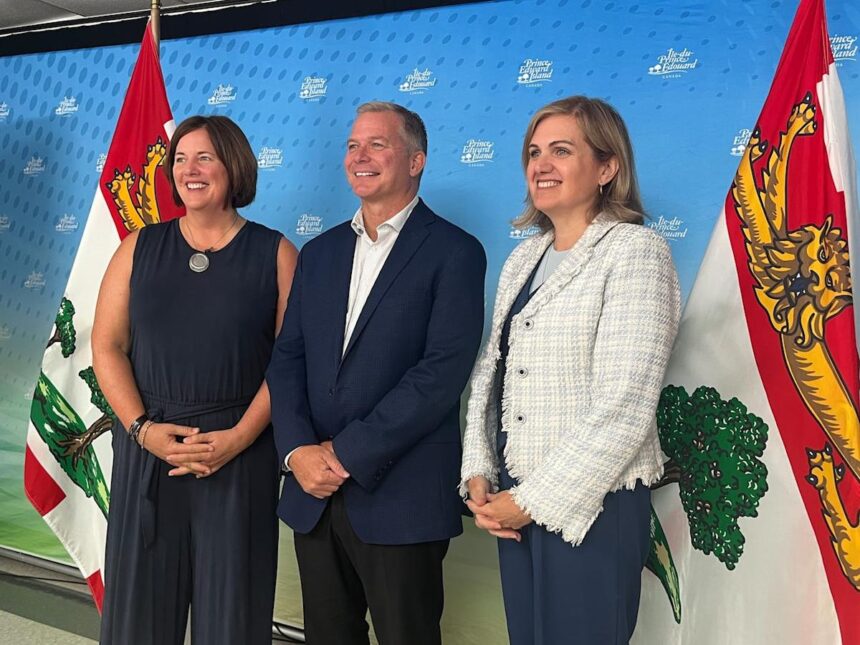
The tension between PEI doctors and the provincial government escalated dramatically this week when Health Minister Mark McLane publicly defended his government’s position amid threats of legal action from the province’s medical society. The dispute centers around a new health-care model that physicians claim was implemented without proper consultation, undermining both doctor autonomy and patient care.
“We have always been committed to working with our doctors,” McLane insisted during a press conference on Wednesday. “But we also have a responsibility to the 35,000 Islanders who don’t have access to primary care.”
The standoff began last month when the provincial government announced plans to implement a new healthcare delivery model that would require physicians to see more patients daily while transitioning some to team-based care settings. Many doctors argue the changes fail to address underlying issues like physician burnout and administrative overload.
According to data from the Canadian Institute for Health Information, PEI has 118 physicians per 100,000 residents – well below the national average of 242 per 100,000. This shortage has created cascading effects throughout the healthcare system, with emergency departments becoming de facto primary care centers for thousands of unattached patients.
“What’s happening in PEI reflects a larger crisis in Canadian healthcare,” explains Dr. Katherine Smart, past president of the Canadian Medical Association. “When governments make unilateral decisions about how care should be delivered without meaningful physician input, it typically backfires – driving more doctors out of the system rather than improving access.”
The Medical Society has given the provincial government until May 15 to address their concerns before pursuing legal options. Their primary demands include meaningful consultation on healthcare reform, recognition of physician autonomy in clinical decision-making, and immediate action on recruitment and retention.
Walking along the Charlottetown waterfront later that evening, I struck up a conversation with Sarah Jeffers, a 42-year-old mother of three who lost her family doctor last year when her physician left the province. “I understand both sides,” she said, watching the sunset over the harbor. “The government needs to fix things, but doctors are people too. They can’t just keep squeezing more and more out of them and expect them to stay.”
Sarah’s experience exemplifies the human cost of this standoff. When her youngest son developed persistent ear infections this winter, she spent eight hours in the emergency room to receive care that would have taken 20 minutes in a family practice. “The whole system feels like it’s unraveling,” she told me.
For McLane, the pressure comes from multiple directions. The province faces a $40 million healthcare deficit, growing waitlists for specialists, and increasing public frustration. “We’re making record investments in healthcare,” he emphasized during Wednesday’s press conference. “But we need to ensure those dollars translate to better access for Islanders.”
However, Dr. James MacDonald, a family physician who’s practiced in Summerside for 27 years, believes the government’s approach misses the mark. “You can’t solve a physician shortage by making the job less attractive,” he explained when I visited his clinic. “Every doctor I know is already working beyond capacity. Adding more patients to our panels without addressing the fundamental issues will only accelerate departures.”
MacDonald’s concerns are supported by a recent survey from Doctors Nova Scotia, which found that 65% of physicians in Atlantic Canada are considering reducing their hours or leaving practice altogether within the next five years. Burnout, administrative burden, and lack of support were cited as primary factors.
The legal threat from the Medical Society represents an unprecedented escalation in doctor-government relations on the island. The society claims the province violated both their negotiated Master Agreement and physicians’ Charter rights by unilaterally changing practice expectations.
Dr. Cassell emphasizes that legal action is a last resort. “We’d much rather be at the table collaborating on solutions than in a courtroom,” she said. “But doctors feel backed into a corner with no other options to protect their practices and patients.”
As evening settles over Charlottetown, the empty clinic I visited earlier serves as a physical reminder of what’s at stake. While government officials and physician representatives exchange increasingly pointed statements, thousands of Islanders continue navigating a fragmented system where basic healthcare access feels increasingly uncertain.
For people like Sarah Jeffers, the technical details of the dispute matter less than its resolution. “I just want my kids to have a doctor again,” she said, pulling her jacket tighter against the spring chill. “I want to know there’s someone who knows their history and who I can call when something goes wrong.”
As both sides prepare for what could be a protracted legal battle, the clock continues ticking on PEI’s healthcare challenges. Whether through negotiation or litigation, the resolution of this dispute will shape healthcare delivery on the island for years to come – and potentially influence similar conflicts brewing across the country.