The taxi meter ticked upward as John Creviston watched the landscape blur past his window. Dense Vancouver Island forests gave way to suburban sprawl and eventually the streets of Victoria – a journey spanning nearly 200 kilometers from his home in Woss. The 81-year-old’s simple medical appointment had triggered what he calls an absurd waste of healthcare resources.
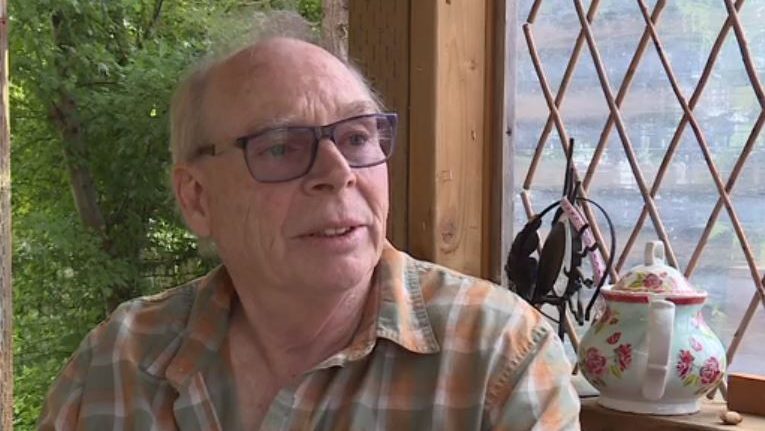
“$1,100 for a taxi ride? This is ridiculous,” Creviston told me when I visited his modest home in the small northern Vancouver Island community. “I could have driven myself and saved the system a fortune.”
Creviston’s story illuminates a growing controversy surrounding Island Health’s patient transportation practices. When the elderly resident needed to visit a Victoria specialist, Island Health arranged and paid for a round-trip taxi ride – costing taxpayers approximately $1,100. The journey took over 2.5 hours each way.
“The taxi driver was nice enough, but he was essentially paid to wait around Victoria for me, then drive all the way back,” Creviston explained, shaking his head. “I’ve lived here 55 years. I can drive myself.”
For residents of remote Vancouver Island communities, accessing specialized healthcare often means significant travel. What’s raising eyebrows isn’t the need to transport patients, but rather the methods and costs associated with Island Health’s approach.
According to the Vancouver Island Health Authority’s financial records, transportation costs have increased by approximately 18% since 2019. The organization spent $5.7 million on patient transportation services last fiscal year, including ambulance services, taxis, and medical transfer vehicles.
Dr. Yasmin Majeed, a health economist at the University of Victoria, points to broader systemic issues at play. “When we examine rural healthcare access, transportation becomes a critical component of the care continuum,” she explained during our interview at her campus office. “The challenge becomes finding cost-effective solutions that don’t compromise patient safety or outcomes.”
Island Health defended their transportation policies in a statement, noting that “patient safety is our primary concern” and explaining that taxi services are utilized when patients cannot safely transport themselves and when medical transfer vehicles are unavailable.
But Creviston’s case isn’t isolated. Catherine Berkhout from Port McNeill shared a similar experience when her 77-year-old mother was transported to Campbell River Hospital via taxi at a cost of approximately $400.
“My mother has a functioning vehicle and a valid driver’s license,” Berkhout said. “When she requested gas reimbursement instead, she was told that wasn’t an option. How does that make financial sense?”
The controversy touches on a deeper tension in British Columbia’s healthcare system: balancing fiscal responsibility with patient needs, particularly in rural communities. The province’s Financial Information Act reports show that healthcare transportation costs across regional health authorities have increased by approximately 23% since 2018.
When I visited Island Health’s administrative offices in Victoria, staff members spoke candidly about the challenges, though most requested anonymity. One program coordinator acknowledged the perception problem: “We understand the optics look bad when high-cost taxis are used, but there are liability issues with patient self-transport that many don’t consider.”
The coordinator explained that reimbursing patients for driving themselves creates potential liability issues if accidents occur. “If we authorize someone to drive themselves and something happens, who bears responsibility?” she asked.
For communities like Woss, population 195, the issue reflects broader rural healthcare challenges. The town’s only clinic operates part-time, with a visiting physician available just two days per week. Specialized care means travel – often significant distances.
Gary Wilson, mayor of the Regional District of Mount Waddington which includes Woss, has been advocating for transportation solutions for years. “Rural communities face a double burden – less access to healthcare and greater travel requirements to receive it,” Wilson explained when I met him at his office in Port McNeill. “But throwing money at expensive taxis isn’t the answer.”
Wilson suggests alternative approaches, such as community volunteer driver programs with appropriate insurance coverage or expanded telemedicine services to reduce unnecessary travel altogether.
Some regions have implemented innovative solutions. Interior Health, for example, operates a Health Connections bus service along set routes to help patients access non-emergency medical appointments in larger centers – at a fraction of taxi costs.
According to Statistics Canada’s 2021 health region data, approximately 19% of Vancouver Island residents live in rural communities, with seniors representing a disproportionately high percentage of these populations. As British Columbia’s population ages, transportation issues will likely intensify.
For Creviston, the issue comes down to common sense. “I’m not saying everyone should drive themselves. Some folks genuinely need assistance,” he said, looking out toward the mountains surrounding his community. “But when you’re paying a taxi driver to sit in Victoria for hours waiting for me, then drive back to a town he probably never heard of before, that’s just poor management of healthcare dollars.”
Island Health has indicated they are reviewing their transportation policies but emphasizes that decisions are made case-by-case, considering patient safety and available resources.
As Creviston shows me his own vehicle in his driveway – a well-maintained sedan he’s driven for years – the irony isn’t lost on either of us. “I’ll be making the same trip next month,” he says. “Wonder if they’ll send another taxi?”
The question hangs in the air, unanswered but pointing toward a healthcare system still searching for the right balance between accessibility, safety, and fiscal responsibility in its approach to rural healthcare.